Time flies when you’re having fun, rite? It’s been approximately six years since I was diagnosed with Type 1 Diabetes. Fun fact, I wasn’t correctly diagnosed at first but I’m backdating this. There is much to say about how many people are misdiagnosed with Type 2, but that’s for smarter people. Type 1 diabetes is a chronic disease I’ll most likely have for the rest of my life and if I don’t treat it with medication (insulin) I will die. Before the discovery of insulin and creating ways for diabetics to get insulin into their bodies, diabetes was a death sentence. I feel very fortunate that today diabetes, while chronic and potentially deadly, is entirely manageable.
For me, and yes this is specific to me because while the basics of diabetes is the same for everyone, how diet, exercise, and medication impact individuals with vary wildly, I have focused on diet and exercise. I’m still dependent on insulin to stay alive, but I do try and keep my insulin intake on the lower side and not boost my dosage to cover diet decisions. Do I occasionally take “glucose excursions” (pasta, ice cream, etc.)? Absolutely. I am human after all. I try to limit my excursions to once a month or so. Travel will also throw me many curveballs so I try and roll with life as it comes.
So, diet and exercise are my two main weapons against diabetes. Exercise does a great job of increasing my sensitivity to insulin, allowing me to take smaller doses to keep my blood sugar under control. I try and do my exercise in the morning so that I have good sensitivity through the day. A nice walk or session on the rowing machine in the afternoon is a big help as well.
For diet, I’ve taken the low carbohydrate route. Yes, I basically given up pasta, bread, rice, cake, cookies, baked goods, and generally anything with wheat or rice flour as a base. So, what’s left? Bacon! The bulk of my macro intake is protein and fat. But, Pat! What about your cholesterol?! It’s fine. I’m pretty lucky to have good genetics for keeping cholesterol under control. Also, the exercise helps out there as well. Keeping processed foods at a minimum is also good, but that’s pretty much good for everybody regardless of your chronic disease status.
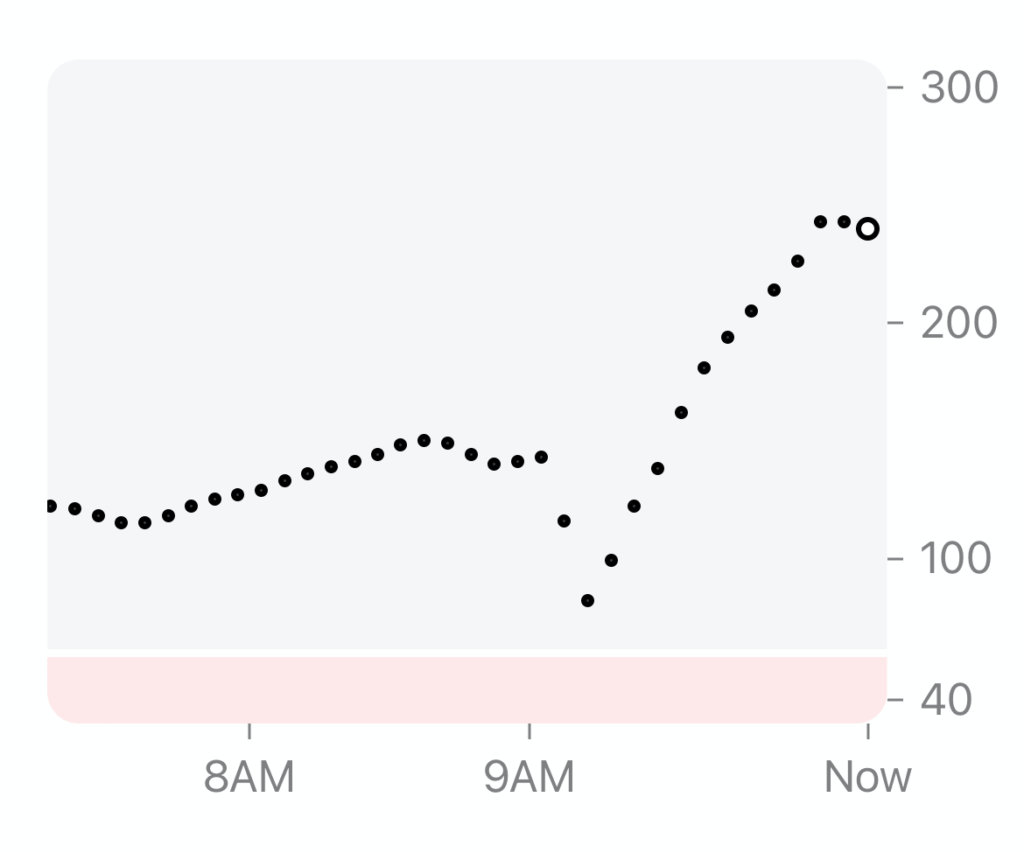
Between diet, exercise, and medication I’ve managed to get my hA1C (the previous gold standard for managing diabetes) down to 5.4. This is the hA1C of a person that does not have diabetes! But hA1C isn’t really something I try and care too much about. It’s a 90-day window measurement and I don’t live in 90-day chunks. I live in 1-day chunks. My CGM allows me to focus on Time In Range (TIR). I strive, on a daily basis to say between 70-180 for my blood glucose levels. Focusing on such shorter time ranges can add unnecessary stress, constantly looking at a number on your phone/watch/device and judging yourself. The diabetes community talks about this quite a bit, and I try to remind myself that it’s just a number and not a judgement about me and my actions. There are over 40 inputs that will impact your blood glucose and diet, exercise, and medication just happen to be the Big Three. Again, smarter people write more eloquently about that topic.
With the recent Apple rumors around non-invasive blood glucose monitoring the whole nerd-o-sphere is talking about diabetes.
So what’s the big deal about invasive blood glucose monitoring? First, it sucks. Second, it sucks. Also, these measurements are a single data point and don’t give directionality. If I do a finger stick and it says 135 (“normal” is 100, but there’s so much complexity there) that’s better than nothing, but I don’t know if it’s going up or down, until I take the next bit of blood and measure. Any time you need to get something from inside your body, there will probably be pain involved.
I’m lucky enough to have the ability to pay, with the “help” of insurance, for continuous glucose monitoring (I’m on the Dexcom G6 and looking forward to the G7). Dexcom is an invasive system, but it’s not actually testing the blood directly. During application of the device a thin filament, not a needle like some folks assume) is inserted under the skin. This filament reacts with the interstitial fluids and derives a blood glucose measurement. The insertion is relatively painless and you only have to do it once every 10 days.
The important thing my Dexcom gives me is directionality since it’s giving me a new reading every 5 minutes. The accuracy is good enough, but probably a little less than getting an actual finger stick reading. Finger stick readings are also less accurate than getting your blood tested in a medical lab. I imagine that the accuracy of rumored Apple technology will be less accurate than most CGM systems.
So in order of accuracy we have medical lab, home finger sticks, CGM, then potential non-invasive technology. I assume this because you’re getting farther away from the actual glucose in the actual blood at each step. I’m also betting that this technology has some serious challenges to be put into a mass market device that doesn’t require a prescription.
You can’t just go buy CGMs off the shelf. They require a prescription because you’re using this data to make decisions about the dosage of medication, in my case it’s insulin. So right there, I doubt any non-prescription system would be able to give an actual number. This is really an FDA problem. A bigger societal problem is that most insurance plans don’t cover CGM for Type 2 diabetes. This is a tragedy as Type 2 can lead to Type 1 and preventing people from becoming Type 1 would be a huge win for everyone.
According to the CDC, 96 million US adults have prediabetes, that is their blood sugar levels are too high. That’s on top of the 37.3 million Americas that already have diabetes.
So why would this non-invasive technology be important? It’s hard to manage what you can’t measure and most people probably don’t want to stick their fingers for blood multiple times a day or wear devices on their bodies for 10 to 14 days at a time. Even if this technology only gave the ability to know when your blood sugar was “above/below normal” would allow folks to, potentially, take action. What kind of action(s)? Exercise and changes in diet. Personally I’ve been able to use these two things to great effect in managing my blood sugar, along with insulin to keep me alive. Non-diabetics experience hypoglycemia and knowing that you needed a little sugar in your system would help you feel better faster.
Again, I have no idea how the FDA will handle this and I know Apple will not want Watch sales restricted by prescription. This makes me thinks that while the rumors are flying, this is at least 5 years out. There’s just too much regulatory red tape to get through. That being said, diabetes tech is getting very, very exciting and I’m hoping it can help people manage this chronic disease.